Treatment for High-Risk Neuroblastoma
Treatment for High-Risk Neuroblastoma
Treatment for High-Risk Neuroblastoma
The intensity of neuroblastoma treatment will vary depending on the risk group assigned to your child’s disease. If your child has high-risk neuroblastoma, you can find information about their treatment in this section. To learn about risk groups overall, you can find information on the Understanding the Treatment Options page.
The treatment goal for children with high-risk neuroblastoma is to prevent neuroblastoma from coming back (relapse). Survival rates are poor for high-risk neuroblastoma patients after relapse, and that’s why the treatment for high-risk neuroblastoma uses multiple intensive therapies.
Multiple therapies are used to treat high-risk neuroblastoma
High-risk neuroblastoma can be aggressive and difficult to treat. It will require intensive treatment with multiple types of therapy. This approach has significantly improved survival rates, and research is now focused on new treatments to further improve survival rates.
See NCCN guidelines for more detailed guidelines.
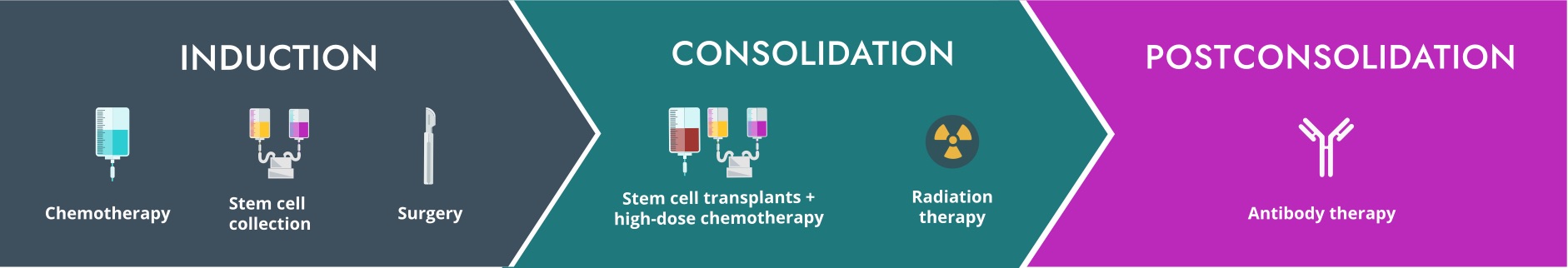
The standard treatment regimen for high-risk neuroblastoma at most hospitals is broken into 3 phases and lasts about 18 months.
Select a topic to learn more about each phase of treatment.
* Please note that some parts of treatment may take place at different hospitals due to need of resources or staffing.Induction
The first phase of your child’s treatment is known as induction. Induction therapy will include multiple cycles of chemotherapy to shrink the tumor and surgery to remove any remaining tumor. Stem cell collection will also happen during this phase. This means your child’s stem cells will be collected and stored for use later in treatment, during the consolidation phase.
Chemotherapy
Chemotherapy is a key part of high-risk neuroblastoma treatment. Chemotherapy medicines stop cancer cells from growing, either by killing the cells or stopping them from dividing and reproducing.
How is the chemotherapy given?
The most common way children with neuroblastoma receive chemotherapy is in their vein through a central line. Learn what a central line is.
 Chemotherapy is a key part of high-risk neuroblastoma treatment.
Chemotherapy is a key part of high-risk neuroblastoma treatment.
Additionally, most chemotherapy for high-risk neuroblastoma will be given in-patient (meaning your child is admitted to the hospital). While your child is in the hospital, a team of oncologists, nurses, and other healthcare professionals help take care of them. Nurses will administer chemotherapy and other supportive medications, monitor for side effects, and support your child 24/7 during hospital admissions.
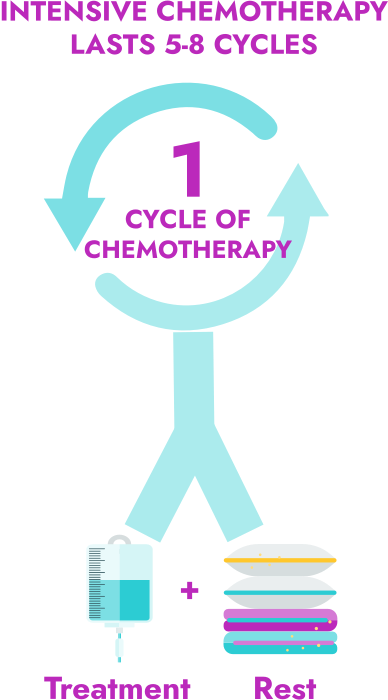
What are chemotherapy cycles?
Induction chemotherapy, like other chemotherapies, will be given in cycles. In this case, your child’s chemotherapy will usually include:
-
5 to 8 cycles of intensive chemotherapy
- 1 cycle of chemotherapy is often close to a month long
- A cycle includes the time that your child is being treated with the chemotherapy as well as the time they are given to rest at home afterward
- For example, if your child receives 1 week of intensive chemotherapy and then 3 weeks of rest without chemotherapy, that makes 1 complete cycle
What chemotherapy medicines will my child receive?
Years of research have shown which chemotherapy regimens work well for high-risk neuroblastoma. Your child’s oncologist will decide which chemotherapy regimens to use based on this research. Medicines that may be a part of your child’s chemotherapy regimen include:
- Topotecan
- Cyclophosphamide
- Cisplatin
- Etoposide
- Vincristine
- Doxorubicin
Speak with your child’s oncologist to learn the specific chemotherapy medicines your child will be given. Depending on the hospital and the severity of your child’s neuroblastoma, the medicines may be used in different combinations and in a different order.
What are the side effects of chemotherapy?
Many of the physical changes or side effects due to chemotherapy are not permanent. It is okay to rely on your child’s healthcare team to figure out how to help manage the side effects, and to talk to your child about some of the changes. Learn more about how to help manage side effects and about supportive care for your child during chemotherapy.
Stem cell collection
What are stem cells and why do they need to be collected?
Stem cells are cells that live in the bone marrow and help the body make new blood cells.
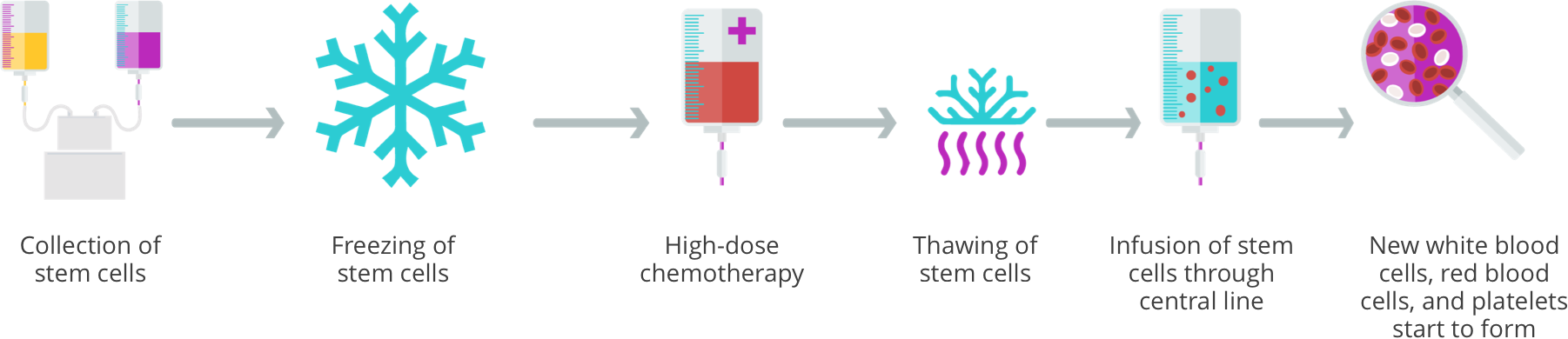
Your child’s oncologist will collect your child’s stem cells during this phase and then freeze them until they are ready for use in the consolidation phase. The stem cells will be infused back into your child through a stem cell transplant. This is done to restore the bone marrow following high-dose chemotherapy (myeloablative chemotherapy).
To help prepare for stem cell collection, oncologists will give children a medicine that helps bone marrow make more white blood cells and helps stem cells move into the bloodstream so they can be collected.
 What are stem cells and why do they need to be collected?
What are stem cells and why do they need to be collected?
How will my child’s stem cells be collected?
The process of collecting your child’s stem cells is known as apheresis.
Oncologists will use a special type of central line to draw blood from your child and pass it through a special machine. This machine will filter out your child’s stem cells and then return the rest of the blood to your child. This process usually takes a few hours and may need to be repeated the following day until enough stem cells are collected. The stem cells are then frozen until the transplant.
Surgery (also called local control)
Surgery will usually occur after a few cycles of chemotherapy so that the tumors are as small as possible and can be easily removed.
During surgery your child’s surgeon will remove any of your child’s visible tumors. This is called resection. The extent of your child’s surgery will depend on the exact location and size of their tumor(s).
- In some cases, a complete removal of your child’s tumor(s) may be possible; this is called complete resection
- If your child’s tumors are in a risky location or wrapped around a large blood vessel, only a partial removal may be possible; this is called partial resection
 Surgery (also called local control)
Surgery (also called local control)
Consolidation
The next phase of your child’s treatment for high-risk neuroblastoma is known as consolidation. The consolidation phase will usually include:
- High-dose chemotherapy (myeloablative) with autologous stem cell transplant
- Radiation therapy
 The next phase of your child’s treatment for high-risk neuroblastoma is known as consolidation.
The next phase of your child’s treatment for high-risk neuroblastoma is known as consolidation.
Just as in the induction phase, the exact treatment your child receives will depend on the treatment plan set forth by their oncologist. Most hospitals now use tandem stem-cell transplant (2 transplants back to back) and radiation therapy for consolidation treatment. In a recent clinical trial, children who had 2 transplants experienced comparable side effects and had lower rates of relapse compared to children who received a single transplant.
The type of transplant that will be used in neuroblastoma is called an autologous stem cell transplant. This process involves giving the child high-dose chemotherapy to kill the cancer cells. This chemotherapy is so strong that it also kills the healthy stem cells in the child’s bone marrow. For this reason, children are always given a stem cell transplant after high-dose chemotherapy to rescue their bone marrow. This is why a stem cell transplant is sometimes called a bone marrow transplant.
Ask your child’s oncologist about the therapies they plan to use as part of your child’s treatment.
Stem cell transplant
What is a stem cell transplant?
You may hear your child’s healthcare team mention stem cell transplant as part of treatment. This process includes both high-dose chemotherapy and autologous stem cell transplant.
How is a stem cell transplant done?
After your child completes high-dose chemotherapy, the child’s frozen stem cells are thawed and given as an infusion through their central line. The stem cells travel through the child’s bloodstream to the bone marrow.
How long will my child be in the hospital for the consolidation phase?
Usually, children will be admitted to the hospital the day before or the day of high-dose chemotherapy and stay until the new stem cells have started making new blood cells. This process usually takes a few weeks, so plan on your child being in the hospital for at least 3 to 4 weeks.
 Radiation therapy
Radiation therapy
Radiation therapy
Radiation therapy kills the neuroblastoma cells by using high-energy rays or particles aimed at a specific area. Radiation may be given to the primary tumor site. Even if the tumor was completely removed, it is possible that a very small (microscopic) amount of tumor was left behind.
Your child’s oncologist may also recommend radiation to sites of metastatic disease (places where disease has spread) that have not completely responded to other therapies.
Common side effects of radiation
Short-term side effects may include:
Postconsolidation (antibody therapy)
The last phase of standard therapy for high-risk neuroblastoma is called postconsolidation or antibody therapy. This phase of treatment will be given after your child’s stem cell transplant and uses monoclonal antibodies, cytokines, and retinoic acid.
Antibody therapy
How does antibody therapy work?
Antibody therapy helps to find remaining neuroblastoma cells that are hiding inside of your child’s body so the immune system can destroy them.
How is antibody therapy given?
Antibody therapy is administered through a vein (intravenously) using the central line.
Most hospitals prefer to give antibody therapy in the hospital. This allows for your child to be monitored by their healthcare team and to receive immediate help if they experience any side effects.
Antibody therapy may be given with other medicines:
- Cytokines to boost the immune system
- A differentiating agent (cis-retinoic acid) to help neuroblastoma cells mature
 How is antibody therapy given?
How is antibody therapy given?
What are the side effects of antibody therapy?
When your child receives antibody therapy, they will also receive premedications (premeds) to help reduce the severity of some side effects. However, some side effects may still occur during antibody therapy. Common side effects may include:
Antibody therapy has greatly improved survival for children with high-risk neuroblastoma and is an essential component to high-risk neuroblastoma treatment.
After your child completes the last phase of high-risk neuroblastoma treatment, it will mark another milestone in your treatment journey. This allows you and your family to start thinking about the future. Once treatment is complete, your child will enter follow-up care, where they will be monitored over the next weeks, months, and years.